Ensuring the highest safety standards in the manufacture of pharmaceutical products is crucial for safeguarding public health. This usually requires both in vitro and animal studies designed to reveal any safety concerns before moving into clinical trials. These tests ensure that pharmaceutical ingredients meet the highest safety standards before reaching consumers. Both in vitro and animal tests are well validated and necessary steps for regulatory approval. However, the findings of a research team led by Professors Bazbek Davletov and Andrew Peden from the University of Sheffield could eradicate the need for animal tests when manufacturing clostridial toxin-based medical products.
Deadly toxins can be used as powerful medicines
Produced by bacteria, clostridium toxins rank among the most dangerous substances known to science. These include the botulinum toxin (the cause of botulism) and the tetanus toxin, both capable of causing fatal paralysis. Yet paradoxically, these same toxins serve as powerful medicines when used in controlled conditions.
Botulinum toxins — also known as Botox — have a wide range of medical applications as well as its better known off-label use in cosmetic procedures. It is used in the treatment of spasticity, and hypersalivation, which affects patients with a range of neurological disorders. Moreover, tetanus toxoid — a modified form of the tetanus toxin — is the backbone of tetanus vaccines, which are administered to 84% of infants worldwide through routine immunisation programs. Tetanus vaccination is also provided to many animals.
The challenge in producing these powerful but potentially dangerous medications lies in safety testing. To avoid deadly consequences, every batch of these pharmaceutical products must undergo rigorous potency, quality and safety testing before reaching patients. The potency testing, a requirement for the registration of pharmaceuticals for human use, has traditionally been assessed using the mouse LD50 lethality assay — a test that determines the dose required to kill 50% of laboratory mice. For tetanus vaccine production, guinea pigs and mice are used in specific toxicity assays mandated by the World Health Organization.
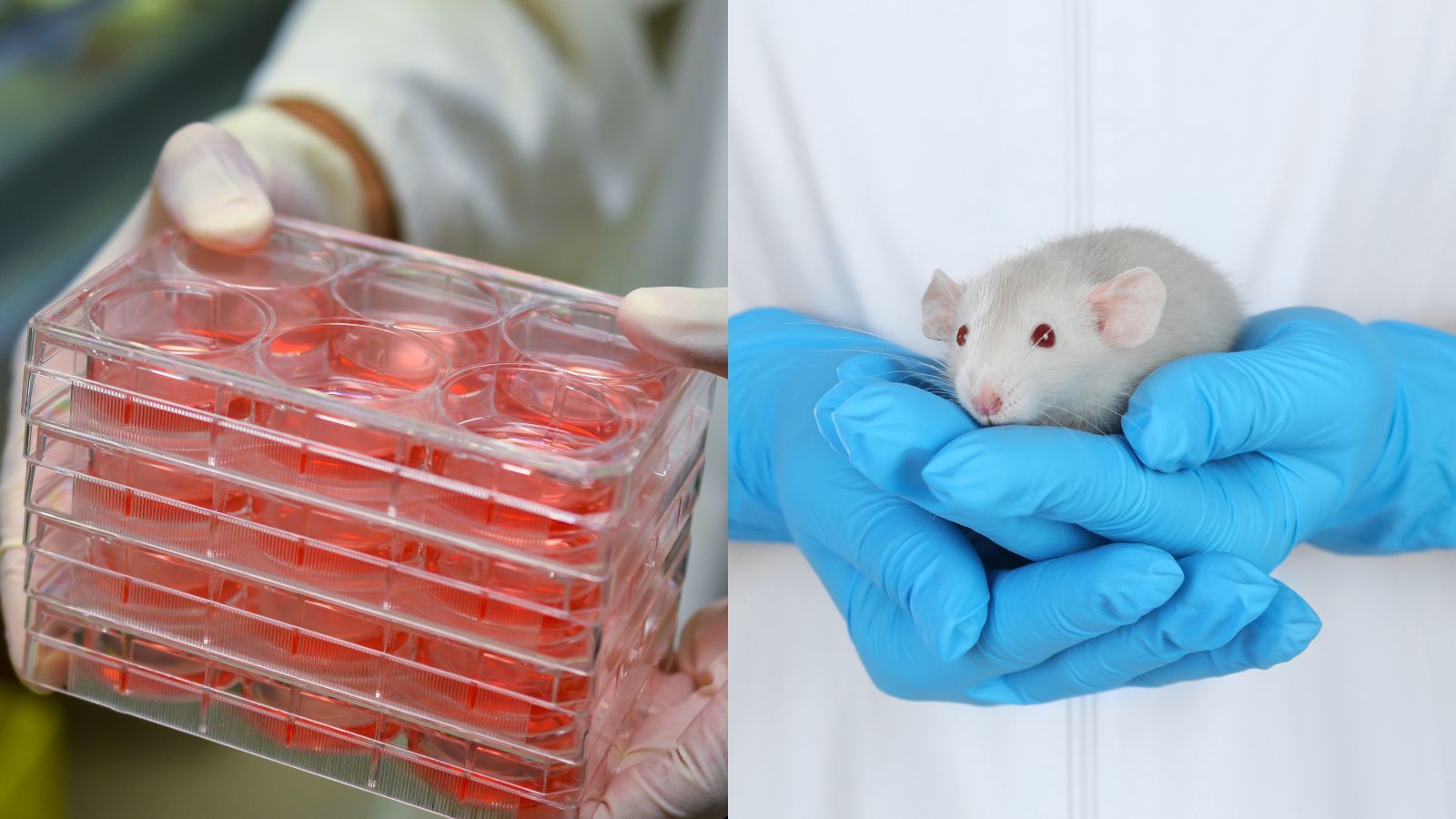
The extensive use of animals for these mandatory tests, along with other drawbacks, have led to the search for alternative and reliable approaches to assess the use of clostridium toxins in medicines.
A new cell-based assay to replace animal toxicity testing
Professors Bazbek Davletov and Andrew Peden, along with their research team at the University of Sheffield, have developed a ground-breaking solution: cell-based assays that could replace animal testing entirely.
Most neuron-like cell lines are not sensitive to tetanus or botulinum toxins as they do not express sufficient levels of the surface proteins the toxins require to bind before they can enter the cells. This has meant that until now, cells on their own couldn’t be used to test the potency of the drugs. However, the Sheffield team engineered human neuroblastoma cell lines that could take up toxins efficiently and replicate the entire intoxication process.
After further refinement, this cell-based system proved remarkably sensitive, allowing the activity of the toxin to be precisely measured. In fact, the assay was shown to be ten times more sensitive to botulinum B toxins than traditional animal testing methods. While the original assay was not sensitive enough to tetanus to fully replace animal testing, further work led to an improved sensitivity to tetanus at the needed physiologically relevant concentrations. This improved non-animal replacement assay has the potential to become a new global gold standard for safety testing of tetanus vaccines.
The impact of this research extends far beyond the laboratory. For any new testing method to succeed in the pharmaceutical industry, it must meet Good Manufacturing Practice (GMP) regulations — the quality standards that govern medicine production. Committing to this goal, ten global tetanus vaccine manufacturers are taking part in studies that will optimise and demonstrate the fitness-for-purpose of these assays. The ultimate objective is to completely replace animal safety tests, a fundamental shift in how we approach pharmaceutical safety testing for these deadly toxins. The success of the Sheffield team's approach could also serve as a template for developing cell-based alternatives to animal testing for other pharmaceutical products.
This collection of research was funded by the UK's National Centre for the Replacement, Refinement and Reduction of Animals in Research (NC3Rs). Read more about it on the NC3Rs website.
Last edited: 3 September 2025 09:25






