Pacemakers – one of the top ten medical inventions?
In 1958, Arne Larsson in Sweden became the first patient to depend on an artificial cardiac pacemaker. He died in 2001 at age 86, having outlived its inventor, the surgeon, and 26 pacemakers.
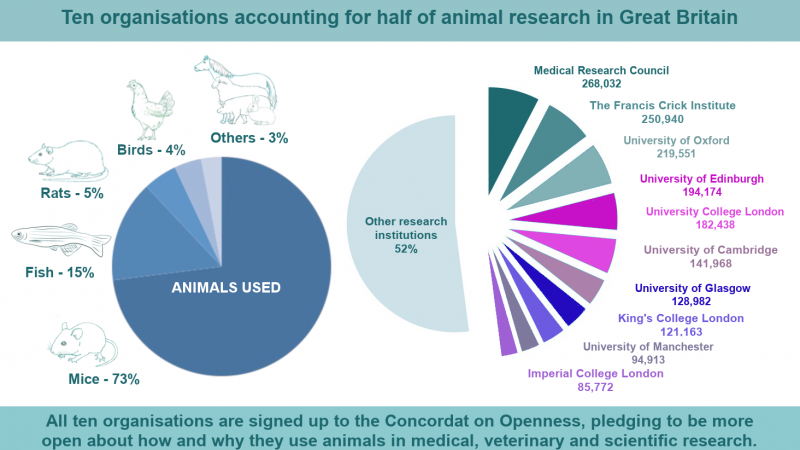
Arne, like the millions of people who have had pacemakers fitted in the last 60 years, benefited from animal research.
Measuring the heart
In 1887 the physiologist Augustus Desire’ Waller working in St. Mary's Hospital, London, recorded the first human surface electrocardiogram using the Lippmann capillary electrometer to deflect a light beam.
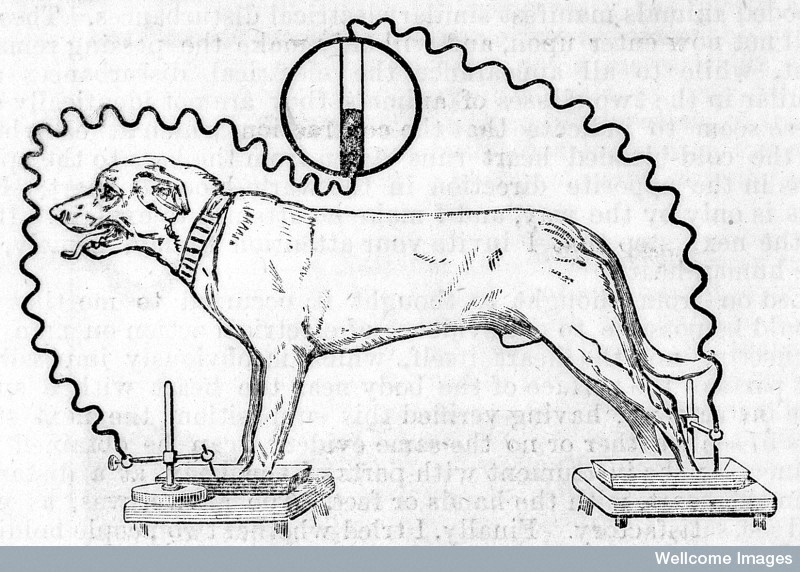
Waller had learnt that “each beat of the heart gives an electric change, beginning at one end of the organ and ending at the other”. He was convinced that he could measure these “electromotive properties of the heart” from the skin surface and proceeded to do so with the electrometer connected between the left and right hands or between the front and back paws of his pet bulldog, Jimmie.
 The ability to record the human (or animal) heart-beat on an electrocardiogram (ECG) developed rapidly and by 1942 the 12 lead electrocardiogram as we know it today had emerged. But the idea of artificially initiating or regulating hearts with electricity was slower to emerge.
The ability to record the human (or animal) heart-beat on an electrocardiogram (ECG) developed rapidly and by 1942 the 12 lead electrocardiogram as we know it today had emerged. But the idea of artificially initiating or regulating hearts with electricity was slower to emerge.
Stimulating the heart
In 1928, the Australian Mark Lidwell In 1928 used intermittent electrical stimulation of the heart to save the life of a child born in cardiac arrest. The child apparently recovered and survived.
In 1932 Albert Hyman became interested in reviving the “stopped heart” by means of “intracardial therapy”. Initially this therapy consisted of the intra-cardiac injection of stimulant drugs such as epinephrine although he soon realised that it was not really the drug that restarted the heart but the needle that set up an action current of injury as it punctured the cardiac wall.
Hyman's invented and named the very first “artificial pacemaker”: it was powered by a spring-wound hand-cranked but did not become accepted as a means of re-starting a stopped heart. However, Hyman did not seem to recognise that his device might have a role for people with heart block.
Electrical conduction system of the heart
The normal electrical conduction in the heart allows the impulse that is generated by the sinoatrial node (SA node) of the heart to be propagated to, and stimulate, the cardiac muscle (myocardium). The myocardium contracts after stimulation. It is the ordered, rhythmic stimulation of the myocardium during the cardiac cycle that allows efficient contraction of the heart, thereby allowing blood to be pumped throughout the body.
In heart block there is damage to the hearts conduction system. This can happen after surgery or with heart disease. Unfortunately, if the natural pacemaker malfunctions, this leads to abnormal heartbeats. These arrhythmias can be very serious, causing blackouts, heart attacks, and even death.
Cardiac surgery on dogs
In 1949 in Toronto, Canada, Wilfred Bigelow and John Callaghan started using hypothermia to reduce metabolism and produce bradycardia and asystole to permit cardiac surgery. Re-warming could not however restore cardiac contraction sufficiently rapidly and so the surgeons started experiments with sino-atrial node stimulation.
In 1949, during an experimental operation on a dog, the heart suddenly stopped. Bigelow recounts: “Out of interest and in desperation, I gave the left ventricle a good poke with a probe I was holding. All four chambers of the heart responded. Further pokes clearly indicated that the heart was beating normally with good blood pressure.” The electric pacemaker was developed as a direct result of these hypothermia experiments.
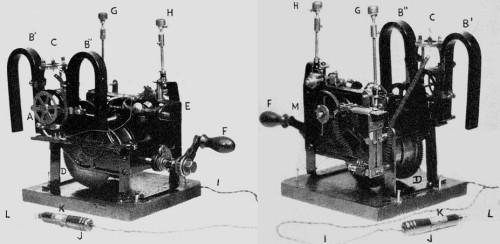
During the 1940's and early 50's the principle device available to generate a variety of electrical impulses, potentially capable of stimulating the heart was an external physiological stimulator manufactured by Grass Manufacturing Co for clinical and physiology lab application.
Clinical cardiac pacing
In 1951 Paul Zoll, a Boston cardiologist, is given credit for ushering in the modern era of clinical cardiac pacing. He developed an external tabletop pacemaker that was successfully applied to the treatment of heart block.
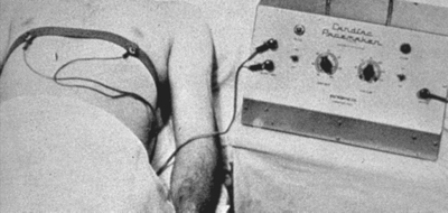
It delivered periodic electric impulses at 2 ms pulse width and 50 to 150 volts alternating current pulse amplitude through a pair of 3 cm2 metal electrodes strapped to the patient's chest directly over the heart. The electrodes irritated the skin and the patients of course found the repeated electric shocks painful.
The mains-powered unit was bulky and heavy and was carried on a cart. It could only go as far as the extension cord would allow.
In 1956 in St. George's Hospital, London, Aubrey Leatham and Geoffrey Davies developed an external stimulator with which to resuscitate patients with heart block and asystole. This mains-powered device stimulated the heart through the intact chest wall utilising 150 volts and was commercially manufactured by Firth-Cleveland in the UK. The commercial version contained several modifications: duration of asystole permitted, sensitivity controls to sense the electrocardiogram, two output ranges and a battery for independent operation.
In 2009 the 500,000th pacemaker operation in the UK took place - at the same hospital, St George's, London, which carried out the first such procedure in 1958. So what were the key developments in the intervening 50 years?
Cardiac surgery and pacing in people
C. Walton Lillehei was a leading cardiac surgeon at the University of Minnesota, Minneapolis and had attained international fame by the mid-50's. Techniques had been developed to enter the heart and correct congenital defects while the circulation was supported. By 1957, Lillehei had performed over 300 open-heart operations on young adults and children.
Despite successful repair of the congenital defect, about 1 patient in 10 developed post-operative complete heart block due to damage of the conducting system while the surgical repair was being performed.
It was thought that temporary rhythm support via pacing would keep the patient alive until natural recovery of the conducting system occurred. The technology developed by Zoll was inappropriate as the high voltage pacing stimuli delivered trans-thoracically would be far too traumatic on these young children.
The physiologist John Johnson proposed the utilisation of the Grass stimulator that was used in the physiology labs to activate hearts. After several experiments, Vincent Gott and William Weirich concluded that a cardiac rhythm could be restored in animal hearts in which heart block had been surgically created by means of a wire inserted into the wall of the right ventricle and connected to the external stimulator. Low voltage pulses at the desired rate could easily stimulate these hearts.
Lillehei and his co-workers developed the myocardial wire: a multi-stranded, braided stainless steel wire in a Teflon sleeve. One end of this was implanted directly into the myocardium and the other end was connected to the physiology lab stimulator. Effective pacing needed only 1.5 volts as there was direct contact with the myocardium. There was no rejection and no damage to the beating heart and the wire could be removed easily by tugging once normal conduction resumed.
The first myocardial wire was implanted on the 30th January 1957 in a 3-year old girl. Pacing was successful and the little girl survived. However, later that year, on October 31st, a municipal power failure lasting three hours resulted in the tragic death of a baby.
The day after, Lillehei requested Earl Bakken to see if his company, Medtronic, could come up with a better device.
Bakkens prototype
Bakken modified a circuit for an electronic metronome, added a mercury battery and control knobs. He recounted,
“Without any grandiose expectations for the device, I was moderately optimistic about what it might eventually do for Lillehei's patients. I drove the device over to the University's animal lab where it could be tested on a dog. Of course it worked.
“The next day I returned to the hospital to work on another project when I happened to walk past a recovery room and spotted one of Lillehei's patients. I must have done a double take when I glanced through the door. The little girl was wearing the prototype I had delivered only the day before! I was stunned. I quickly tracked down Lillehei and asked him what was going on. In his typical calm, measured, no-nonsense fashion he explained that he’d been told by the lab the pacemaker worked and he didn’t want to waste another minute without it. He said he wouldn’t allow a child to die because we hadn’t used the best technology available.”

Lillehei with a child being paced
1958: First implantable pacemaker
On October 8th, 1958 the first pacemaker implantation was performed in Sweden. The system had been developed by the surgeon Ake Senning and the physician inventor Rune Elmqvist and implanted on a 43-year old engineer called Arne Larsson.
Arne suffered from Stokes-Adams attacks that required resuscitation many times daily and whose situation was considered hopeless. The implantation was a desperate attempt to save him.
Senning and Elmqvist realised that the main problem with external pacemakers was the open route for infection along the lead and decided to design a fully implantable system.
Senning recounts his encounter with Else Marie Larsson, Arne’s wife: "An energetic, beautiful woman entered my lab on the 6th October 1958 and told me that I had to implant a pacemaker into her husband. I told her we had not completed our experimental series and we did not have a pacemaker for human clinical implantation. She demanded: ‘So make one!’.
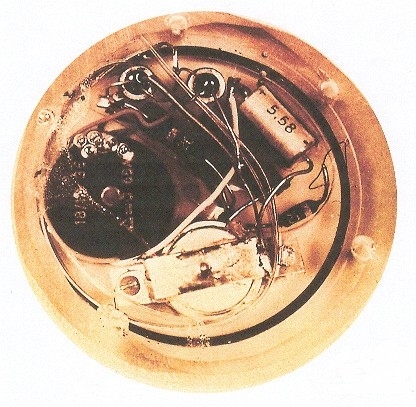
The pacemaker
The entire unit was entirely hand-made and consisted of the nickel-cadmium batteries, the electronic circuit and the coil recharging antenna. These were encapsulated in a new epoxy resin (Araldite) produced by Ciba-Geigy, which had excellent biocompatibility. The approximate diameter and thickness became 55 mm and 16 mm respectively, according to the dimensions of the ever so popular shoe polish can from Kiwi. Elmquist in fact produced two such units using these cans as moulds!
Meanwhile – back in the US
Wilson Greatbatch was an electrical engineer teaching at the University of Buffalo where he was working on an oscillator to aid in the recording of tachycardias. He accidentally discovered the way to make an implantable pacemaker circuit when he wired in the wring value resistor and started an oscillation with 1.8 millisecond pulse followed by a 1 second interval.
He persuaded Dr. William Chardack chief of surgery at Buffalo's Veteran's Hospital of its utility and shortly afterwards Chardack and another surgeon, Dr. Andrew Gage, exposed the heart of a dog in the hospital animal lab to which they touched the two pacing wires. The heart proceeded to beat in synchrony with the device.
After another two years of experiments with animals the first human operation took place on June 1960 on a 77-year old man in complete heart block. The patient went on to live another two years.
50 years of improvements
Various problems with batteries, leads and casing and surgical techniques were steadily overcome over the next decade with models not unlike present day pacemakers becoming available in the 1970s. The need for batteries was avoided in some models entirely by using an external power source to induce activity in an internally placed circuit.
Now pacemakers can respond to the bodies demand in a sophisticated manner with automatic adjustment of stimulation amplitude reducing power use and extending the battery life to as much as 8 years.
Next steps
Currently trials are under way with tiny pacemakers, the size of a large pill. These can be placed directly into the heart intravenously and receive their power from an external source.

Further into the future it might be possible to biologically repair damaged hearts with heart stem cells set on the track to make conductive tissue. Trials with pigs are investigating this possibility.
In any event, today’s technology is keeping around 250,000 people in the UK in better health, part of the 4 million plus worldwide fitted with a pacemaker.
The pacemaker is an electronic biomedical device that can regulate the human heartbeat when its natural regulating mechanisms break down. It is a small box surgically implanted in the chest cavity and has electrodes that are in direct contact with the heart. It is used to treat some abnormal heart rhythms that can cause your heart to beat too slowly or miss beats. Some pacemakers can also help the chambers of your heart beat in time.
Pacemaker facts
- More than 1 000 000 pacemakers and more than 200 000 defibrillators are implanted in the world each year
- The global market revenue for pacemakers in 2012 was $4.3bn
- After a pacemaker exploded in a crematorium, causing an unpleasant surprise and damaging brickwork – pacemakers are removed from the body before cremation.
- The charity http://www.pace4life.org arranges the re-use of pacemakers
- In the United Kingdom, approximately 35,000 individuals receive pacemaker each year, costing around £5,000 - £15,000 a time.
- Pacemakers are not generally a problem when going through airport security
- Pacemakers have been inserted into 5 days old babies and into adults aged over 100
- Pacemakers are not visible from then outside except for a small scar, usually under the collar-bone, where the pacemaker is inserted.
- Batteries last for years because the heart only needs to be stimulated with a small current.
- When the batteries run low a new battery is fitted
- People can do usual activities after having a pacemaker fitted including having sex
- A pacemaker is about the size of a small box of matches
- Pacemakers with radioactive batteries were made because of the long battery life, but are not made now.
References
-
Main reference: A brief history of cardiac pacing http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232561/
- https://www.bhf.org.uk/heart-health/treatments/pacemakers
- http://news.bbc.co.uk/1/hi/health/8012420.stm
- http://www.pace4life.org/
- http://www.madehow.com/Volume-3/Pacemaker.html#ixzz3hk9q3tSz
- http://www.sscts.org/pages/historypacemakers.aspx
- http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232561/
- http://www.businessinsider.com/r-gene-therapy-creates-biological-pacemaker-cells-for-the-heart-2014-16?IR=T
- http://stm.sciencemag.org/content/6/245/245ra94
- http://www.medtronic.com/innovation/smarter-miniaturization.html
- http://www.madehow.com/Volume-3/Pacemaker.html#ixzz3hkAMdv7N
Last edited: 3 October 2023 09:43